Insulin resistance is a common but often misunderstood condition that plays a major role in a range of chronic health problems—including prediabetes, type 2 diabetes, cardiovascular disease, and obesity. It can develop silently over many years, making awareness and early intervention key to protecting your long-term health.
What Is Insulin Resistance?
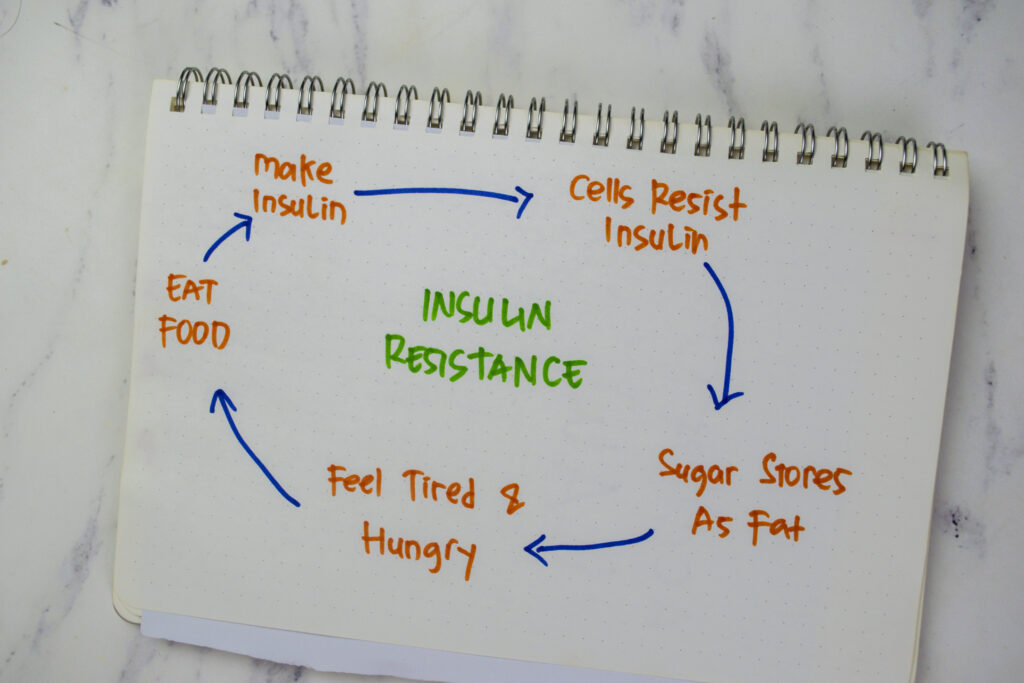
Insulin is a hormone made by the pancreas that helps transport glucose (sugar) from the bloodstream into your body’s cells to be used for energy. Insulin resistance occurs when the body’s cells become less responsive to insulin. As a result, the pancreas produces more insulin to compensate and keep blood sugar levels stable.
Over time, this compensation may no longer be effective, leading to elevated blood sugar levels and the development of prediabetes or type 2 diabetes.
Common Symptoms of Insulin Resistance
In its early stages, insulin resistance may not cause any obvious symptoms. However, some people may experience:
- Fatigue, especially after eating
- Increased hunger or sugar cravings
- Weight gain, especially around the abdomen
- Difficulty losing weight
- Darkened patches of skin (acanthosis nigricans), often on the neck or underarms
- Irregular menstrual cycles or signs of PCOS (polycystic ovary syndrome) in women
Because these symptoms can be vague, many people remain undiagnosed until more serious health issues develop.
How Is Insulin Resistance Diagnosed?
There is no single test to diagnose insulin resistance directly, but healthcare providers use a combination of tests and clinical markers to assess insulin function and metabolic health:
- Fasting glucose and insulin levels
- Hemoglobin A1C (reflects average blood sugar over 2–3 months)
- HOMA-IR (a calculated score based on fasting glucose and insulin)
- Lipid panel (often shows high triglycerides and low HDL)
- Oral glucose tolerance test (OGTT)
Your healthcare provider may also consider body weight, waist circumference, blood pressure, and family history when evaluating insulin resistance.
Health Implications of Insulin Resistance
Insulin resistance is a key driver of metabolic syndrome, a cluster of conditions that includes high blood pressure, elevated blood sugar, abnormal cholesterol levels, and excess abdominal fat. Left unaddressed, insulin resistance increases the risk for:
- Type 2 diabetes
- Heart disease
- Non-alcoholic fatty liver disease (NAFLD)
- Polycystic ovary syndrome (PCOS)
- Dementia and Alzheimer’s disease
- Certain cancers (e.g., breast, colorectal)
Early detection and intervention are critical to preventing these long-term complications.
Treatment Options
1. Lifestyle Modifications
Lifestyle change is the cornerstone of managing insulin resistance and improving insulin sensitivity:
- Nutrition:
Focus on a balanced, lower-glycemic diet rich in whole foods, including:
- Non-starchy vegetables
- Lean proteins
- Healthy fats (e.g., olive oil, nuts, avocado)
- Whole grains in moderation
- Avoid or reduce added sugars, refined carbohydrates, and processed foods.
- Exercise:
Regular physical activity improves how your body uses insulin. Both aerobic exercise (like walking, swimming, cycling) and resistance training (like weightlifting or bodyweight exercises) are beneficial. Aim for:
- At least 150 minutes of moderate activity per week
- Strength training 2–3 times per week
- Weight loss:
Even modest weight loss (5–10% of body weight) can significantly improve insulin sensitivity and reduce the risk of developing type 2 diabetes. - Stress management and sleep:
Chronic stress and poor sleep can worsen insulin resistance. Prioritize 7–9 hours of quality sleep per night and engage in stress-reducing practices like mindfulness, yoga, or therapy.
2. Medications
For some individuals, lifestyle changes alone may not be enough, and medications may be helpful:
- Metformin: A first-line medication that improves insulin sensitivity and lowers blood glucose.
- GLP-1 receptor agonists (e.g., semaglutide, terzepatide, liraglutide): Help regulate blood sugar, promote weight loss, and improve insulin response.
- Thiazolidinediones (e.g., pioglitazone): Improve insulin sensitivity in fat and muscle tissues.
- Inositol supplements (especially in women with PCOS): May support insulin signaling in some cases.
Treatment plans should be personalized based on your individual risk factors, goals, and health conditions.
Long-Term Health Risks
If left untreated, insulin resistance can progress to chronic illnesses that significantly affect quality of life and increase the risk of disability or early death. These include:
- Type 2 diabetes
- Cardiovascular disease (heart attack, stroke)
- Kidney disease
- Vision loss (from diabetic retinopathy)
- Nerve damage
- Increased cancer risk
The good news is that insulin resistance is reversible—especially when caught early. Making informed, sustainable changes now can reduce or even eliminate future health risks.
Final Thoughts
Insulin resistance is not just a warning sign—it’s a clear opportunity for prevention and empowerment. With the right support, many people can improve insulin sensitivity, lose weight, reduce their risk of chronic disease, and feel better overall.
If you suspect you might be insulin resistant or are struggling with weight gain, fatigue, or blood sugar issues, talk to your healthcare provider. Early action makes all the difference.